Transforming Respiratory Services
The aim of this project was to transform the Highland Respiratory Care pathway towards a pathway that is truly patient centred, by co-designing it with patients and all those who either use or provide respiratory services from the outset.
Our project team comprised of:
- NHS Highland’s Technology Enabled Care (TEC) team
- University of Highlands & Islands (UHI), Division of Rural Health and Wellbeing
- A medical research doctor embedded in the Respiratory Service
Our stakeholder group included:
- Patient & carer representatives
- Chest Heart and Stroke Scotland
- LGOWIT (Let’s Get On With It Together)
- Respiratory specialists including consultants, nurses and physiotherapists
- Primary Care representatives, including GPs
- Public Health and IT specialists from NHS Highland
- Scottish Ambulance Service
- Housing organisations
- Scottish Government
The Journey
Project Set Up: May 2019 – October 2019
Recruitment of researchers and a project manager, research ethics approval, building relationships between partners, project planning and a first pathway mapping exercise.
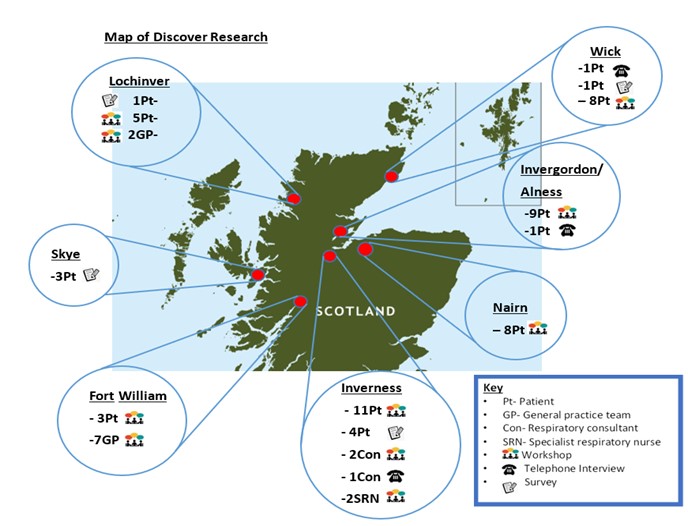
Discover Phase: November 2019 – April 2020
During our Discover phase, we wanted to explore the end-to-end life circumstances and journey for people who experience respiratory symptoms. We designed and carried out a range of research activities with stakeholders, in total engaging with over 120 people. These included:
- Workshops across the Highlands run by researchers from UHI
- Informal interviews, questionnaires and discussion groups run by TEC researchers
Map of Discover Phase Research
In addition, we:
- Undertook a literature review, collating findings from secondary sources
- Heard about findings from research undertaken by third sector organisations & housing
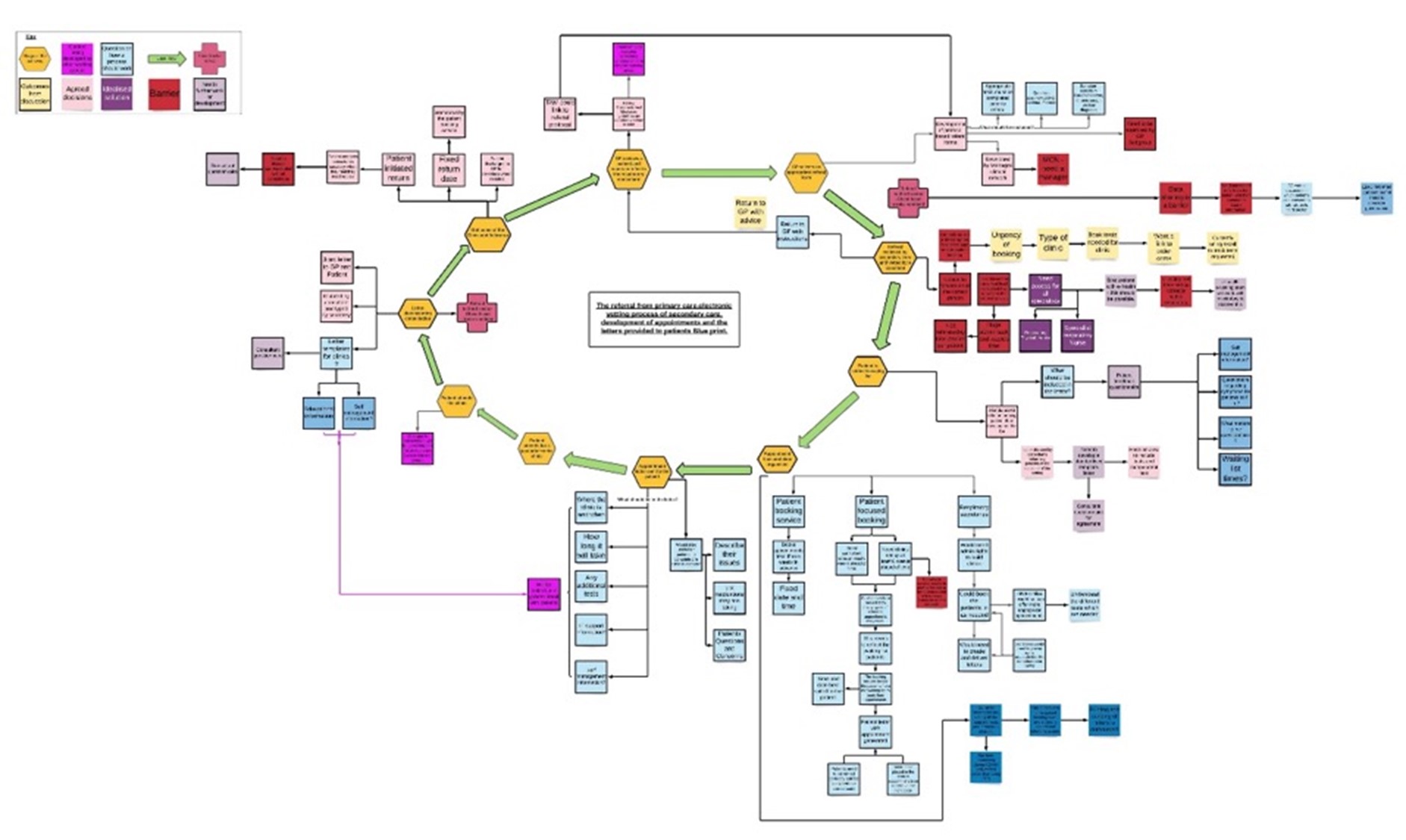
As a result of this work we understood far more about the respiratory pathway as experienced by both patients and healthcare staff, and developed a far more complex diagram of our system than we had originally envisaged:
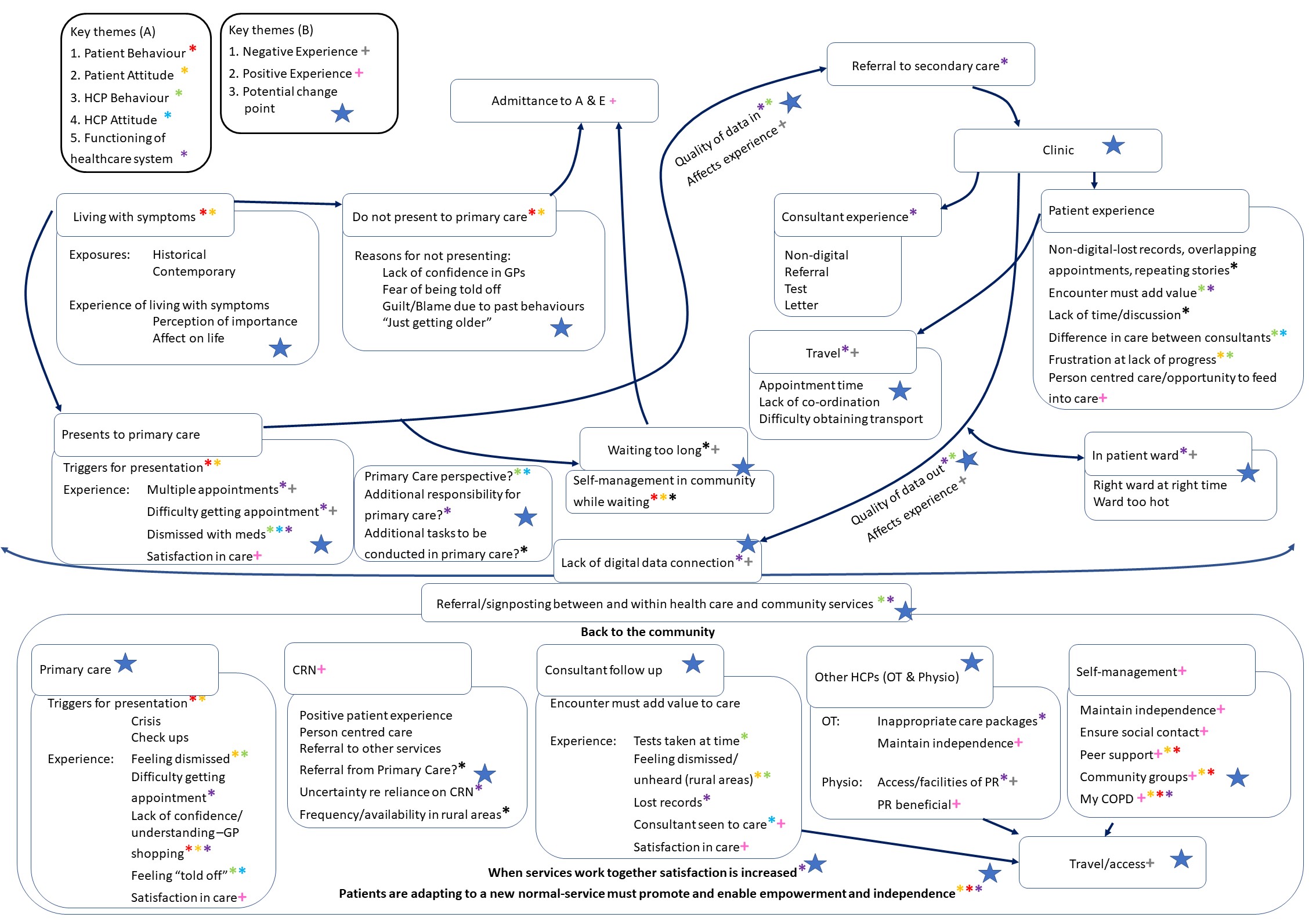
Define Phase: May 2020 – October 2020
After analysing our research findings, during the Define phase we brought together findings from all our different sources, triangulated the findings, identified key patient needs and problem statements, prioritised issues, and looked at the feasibility of addressing them. Additional research with patients to prioritise issues was also undertaken.
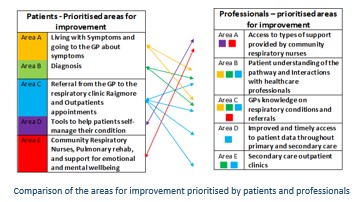
From this work we developed our overarching problem statement:
Develop Phase - Ideation: November 2020 – June 2021
We started our work to Develop solutions to the problems we had identified by sending out questionnaires, and holding individual stakeholder workshops and a well-attended joint stakeholder workshop (November 2020), and we continued our work in a set of three short-life working groups, which each met monthly during January to June 2021. These working groups were extremely well attended and included ideation sessions, guided discussions, and the use of blueprints, prototypes and storyboards.
An extensive range of fact finding meetings were also required, with a range of NHS Highland staff, the ambulance service, third sector organisations and commercial suppliers.
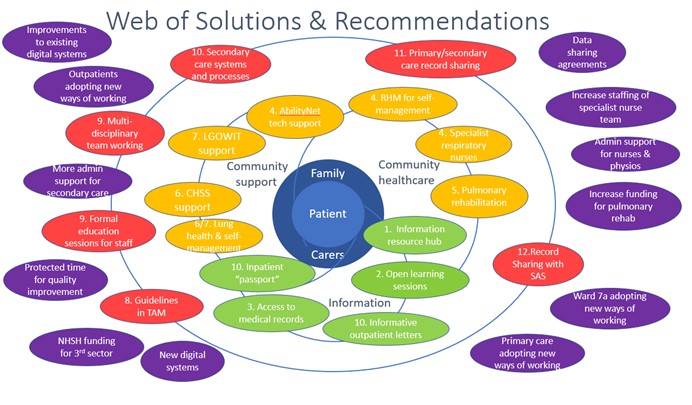
One result of this first part of the develop phase was a report prepared for NHS Highland’s Board, setting out our findings and recommendations for change.
Develop Phase - Prototyping: July 2021 – March 2022
This second part of the develop phase involved detailed work on developing, prototyping and testing our ideas, working in collaboration with a variety of stakeholders, liaising with others, exploring options, writing papers, negotiating, seeking approvals, and much more.
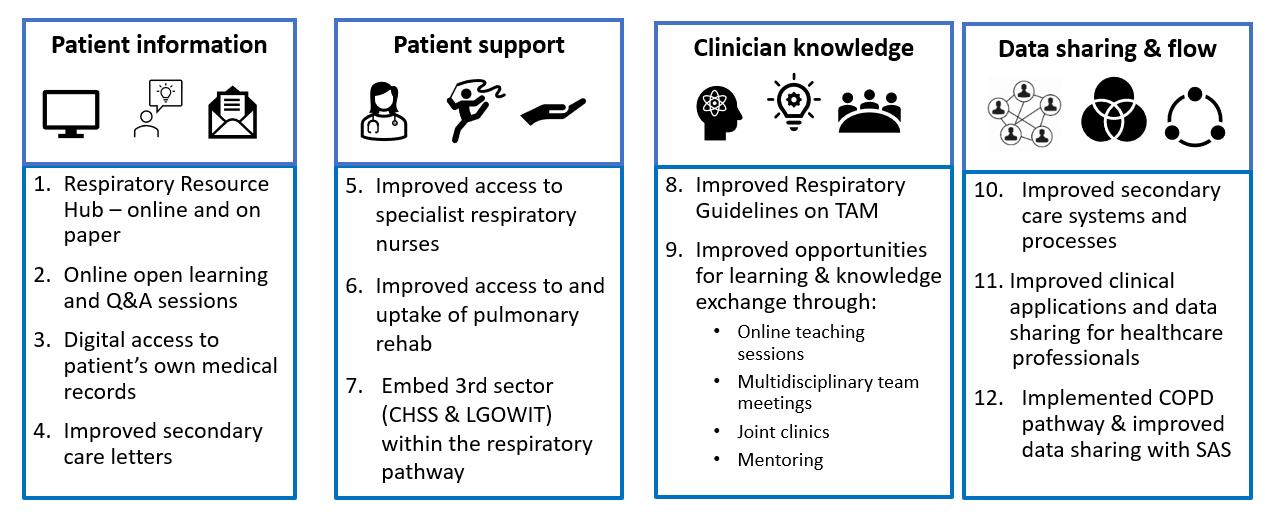
Our focus was on four main areas of change, comprising 12 individual workstreams, some of which had multiple strands:
- Improving patients’ access to information – through development of a respiratory resource hub, a programme of open learning sessions, digital access to health records and improved secondary care letters.
- Improving patients’ access to support – especially through supporting, developing and standardising the specialist respiratory nurse and pulmonary rehab services, while also working to embed our 3rd sector organisations (CHSS and LGOWIT) within the respiratory pathway
- Improving clinicians’ knowledge and understanding of respiratory conditions and when to make referrals to secondary care – through improvements to respiratory guidelines, online teaching sessions and formalising multidisciplinary team working, including MDT meetings about complex cases, joint clinics and mentoring.
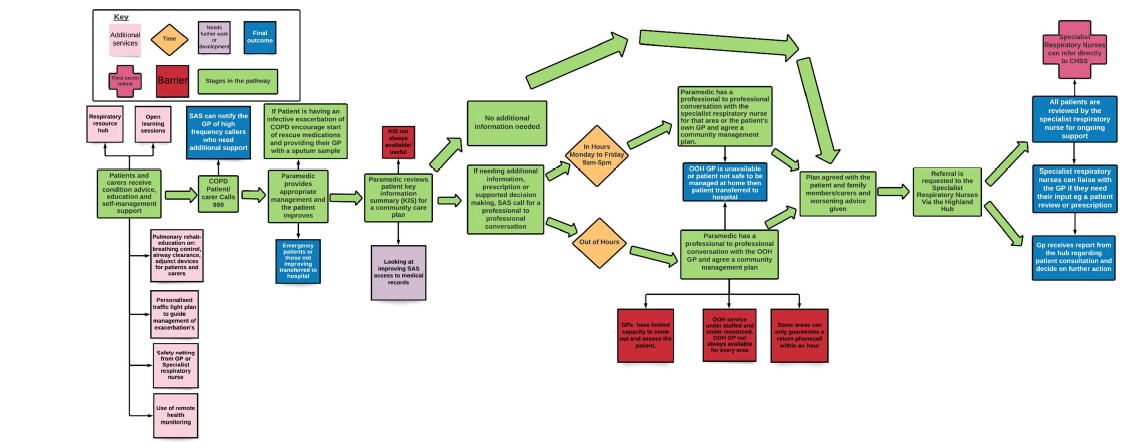
- Improving processes, systems, data sharing and flow – through improvements to and standardisation of secondary care processes, improvements to clinical applications, implementation of the Scottish Ambulance Service (SAS) COPD pathway, and improvements to data sharing between primary care, secondary care and the ambulance service.
Deliver Phase: November 2021 – September 2022
The final phase of the project involved delivery of new and improved services. Our first solution went live at the beginning of November 2021, with others going live in February, April and September 2022. In each case, the solutions have been continuously evaluated and developed based on participant feedback and PDSA cycles.
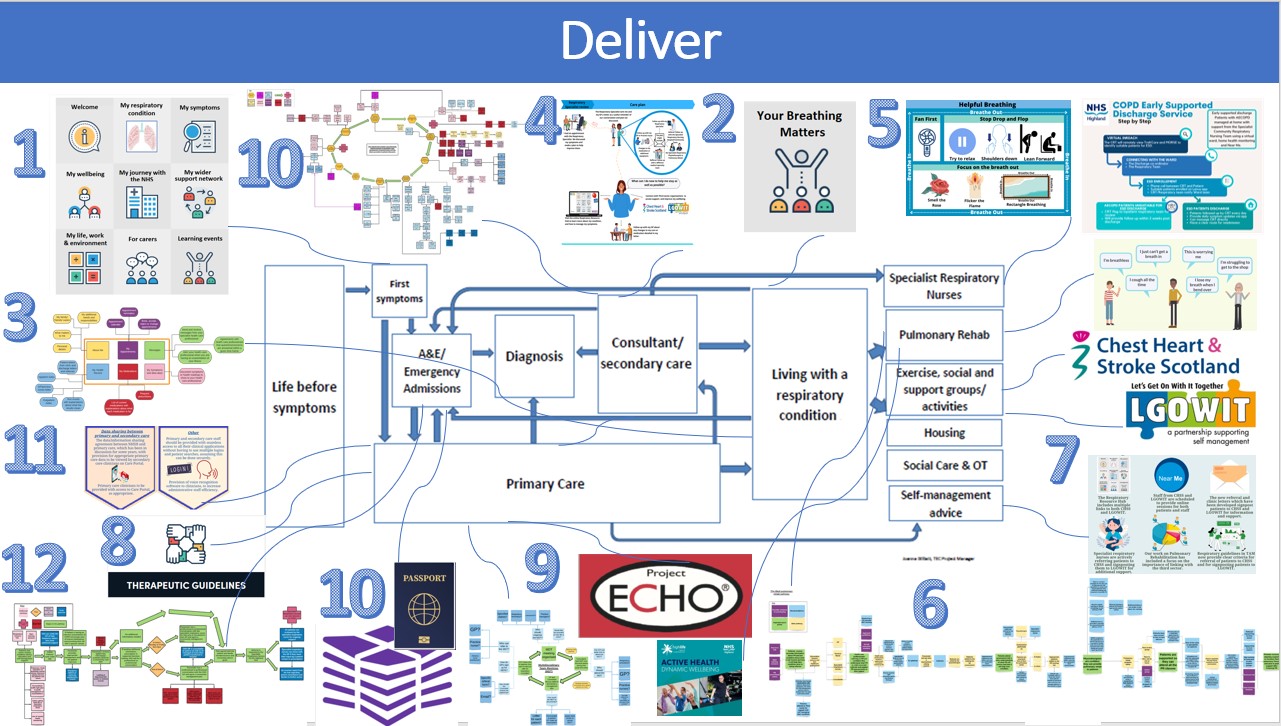
Although we are encountering a number of bumps in the road, we are making progress towards implementation of all of these solutions, and seven of them are now up, running and in use.
1. Respiratory Resource Hub: A website which provides easy access to information for respiratory patients and carers by bringing together links to existing information provided by trusted sources, plus providing some locally produced content.

2. Your Breathing Matters: Online learning sessions to provide easy access to education on respiratory conditions and symptoms, self-management advice and wider non-medical information relating to respiratory health (e.g. housing).
3. Digital Access: The TEC team and respiratory colleagues are continuing to work with DHI and eHealth, to help design a Digital Access solution, and then to run a pilot or test of change.
4. Secondary Care Letters: New letter have been designed, to be sent to patients on receipt of their referral and after clinic appointments. To be trialled as soon as pressures on the respiratory service allow.

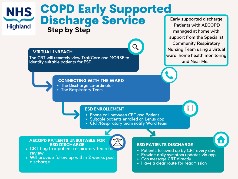
5. Access To Specialist Respiratory Nurses: Building on the pathfinder’s work, Interface Care funding is now being used to support a new Early Supported Discharge service, virtual ward, remote monitoring, an admin coordinator and an additional nurse.
6. Access To And Uptake Of Pulmonary Rehab: Development of pulmonary rehab is now being taken forward by NHSH’s new Rehabilitation Steering Group. High Life Highland have launched Active Health classes suitable for respiratory patients and we have developed an animated promotional video.

7. Embed 3rd Sector In The Pathway And Solutions: Our work has actively incorporated the 3rd sector, involving them in the design & development of our solutions, and promoting their services within our other solutions.

8. Improved Respiratory Guidelines in TAM: We identified gaps, then drafted and refined new or improved guidelines to aid diagnosis, management and referral of respiratory patients and signposting to additional information and support.

9. Improved Opportunities For Clinician Learning And Knowledge Exchange: Following an educational needs assessment, we developed a course of ECHO sessions for primary care, the first course was delivered and more are planned. We also plan to formalise MDT working clinical commitments allowing.

10. Improved Secondary Care Systems And Processes: We explored the current pathways and systems in place for offering patient appointments and for provision of support services for inpatients. However, it was not possible to make changes to either within the timescale of the project.
11. Improved Clinical Applications and Data Sharing: We worked extensively with the respiratory professionals and senior eHealth staff to identify issues and areas for possible improvement. Some issues were addressed and eHealth will continue to work on others.
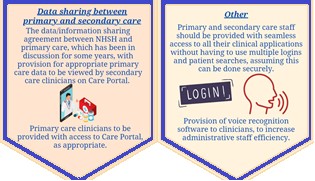
12. Improved Data Sharing With SAS: We successfully implemented the new SAS COPD pathway, with agreement for patients not transferred to hospital to be followed up within the community. We also prompted national discussions of data sharing between NHS & SAS.
For more information about our project please visit:
Discover and Define – www.bit.ly/DiscoverPadlet
Develop and Deliver – www.bit.ly/RespiratoryPathfinder
Contacts – to find out more
Rowena Cooper - rowena.cooper6@nhs.scot
Joanna Gilliatt - joanna.gilliatt@nhs.scot
